Case of Heart Failure
Case of Heart Failure
Prof. Dr. Soliman Ghareeb ,MD.
Professor of Cardiovascular Medicine Cairo University
Management of DHF
. Reduce symptoms
. Control hypertension
. Prevent myocardial ischemia
. Diuretics – provide the most symptoms relief if fluid retentionn is a future
. ACE inhibitors and β Blockers – complement diuretics well
. Central sympatholytics – hypertensive episodes
. Nitrates – preventing ischemia
. Trimetazidine – as a metabolic support
Did they apply the guidelines recommendation?
2013 ACCF/AHA Guideline for the Management of Heart Failure
. Developed in Collaboration With the American Academy of Family Physicians, American College of Chest Physicians, Heart Rhythm Society, and International Society for Heart and Lung Transplantation
. Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation
. American College of Cardiology Foundation and American Heart Association, Inc.
|
Classification |
Ejection Fraction |
Description |
|
I. Heart Failure with Reduced Ejection Fraction (HFrEF) |
≤40% |
Also referred to as systolic HF. Randomized clinical trials have mainly enrolled patients with HFrEF and it is only in these patients that efficacious therapies have been demonstrated to date. |
|
II. Heart Failure with Preserved Ejection Fraction (HFpEF) |
≥50% |
The diagnosis of HFpEF is challenging because it is largely one of excluding other potential noncardiac causes of symptoms suggestive of HF. |
|
a. HFpEF, Borderline |
41% to 49% |
These patients fall into a borderline or intermediate group. Their characteristics, treatment patterns, and outcomes appear similar to those of patient with HFpEF. |
|
b. HFpEF, Improved |
>40% |
It has been recognized that a subset of patients with HFpEF previously had HFrEF. These patients with improvement or recovery in EF may be clinically distinct from those with persistently preserved or reduced EF. Further research is needed to better characterize these patients |
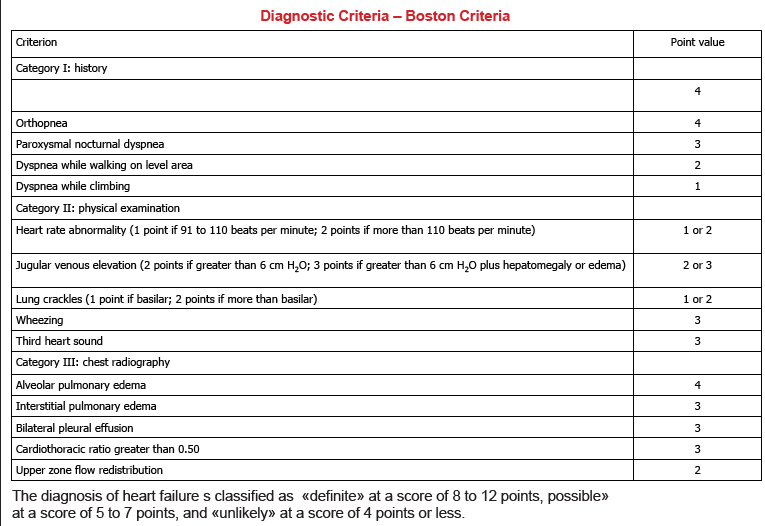
Initial and Serial Evaluation of the HF Patient Clinical Evaluation
Definition of Heart Failure
Initial and Serial Evaluation of the HF Patient
History and Physical Examination
A thorough history and physical examination should be obtained/performed in patients presenting with HF to identify cardiac and noncardiac disorders or behaviors
that might cause or accelerate the development or progression of HF.
Initial and Serial Evaluation of the HF Patient
Diagnostic Tests
Initial laboratory evaluation of patients presenting with HF should include
1- complete blood count,
2- urinalysis,
3- serum electrolytes
4- blood urea nitrogen, serum creatinine,
5- glucose, fasting lipid profile, liver function tests, and thyroid-stimulating hormone.
Serial monitoring, when indicated, should include
serum electrolytes and renal function.
. A12-lead ecg should be performed initially patients presenting with HF.
diagnostic tests for rheumatologic diseases amyloidosis,
Classification of Heart Failure
|
ACCF/AHA Stages of HF |
NYHA Functional Classification |
|
|
At high risk for HF but without structural heart disease or symptoms of HF. |
None |
|
|
Structural heart disease but without signs or symptoms of HF. |
I |
No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF. |
|
Structural heart disease with prior or current symptoms of HF. |
I |
No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF. |
|
II |
Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in symptoms of HF. |
|
|
III |
Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes symptoms of HF. |
|
|
Refractory HF requiring specialized interventions. |
IV |
Unable to carry on any physical activity without symptoms of HF, or symptoms of HF at rest. |
Initial and Serial Evaluation of the HF Patient
History and Physical Examination
A thorough history and physical examination should be obtained/performed in patients presenting with HF to identify cardiac and noncardiac disorders or behaviors
that might cause or accelerate the development or progression of HF.
Initial and Serial Evaluation of the HF Patient
Diagnostic Tests
Initial laboratory evaluation of patients presenting with HF should include
1- complete blood count,
2- urinalysis,
3- serum electrolytes
4- blood urea nitrogen, serum creatinine,
5- glucose, fasting lipid profile, liver function tests, and thyroid-stimulating hormone.
Serial monitoring, when indicated, should include
serum electrolytes and renal function.
. A12-lead ecg should be performed initially patients presenting with HF.
diagnostic tests for rheumatologic diseases amyloidosis
or pheochromocytomq are reasonable in patients presenting whith hf in whom there is a clinical suspicion of these diseases.
Biomarkers
Ambulatory/Outpatient
measurement of BNP or NT-probnp is useful for establishing diagnosis and prognosis or disease serverity in chronic HF.
. BNP
- 001<high negative predictive value
- 004> consistent with HF
- A.fib, chronic HF, pulmonary HTN, renal
failure " higher at baseline, so use higher cut-off for dx of acute diastolic heart failure
- Lower in obese people at baseline, so use lower cut-off for dx of acute diastolic heart failure
biomarkers of myocardial injury my be considered for additive risk stratification in patients with chronic HF.
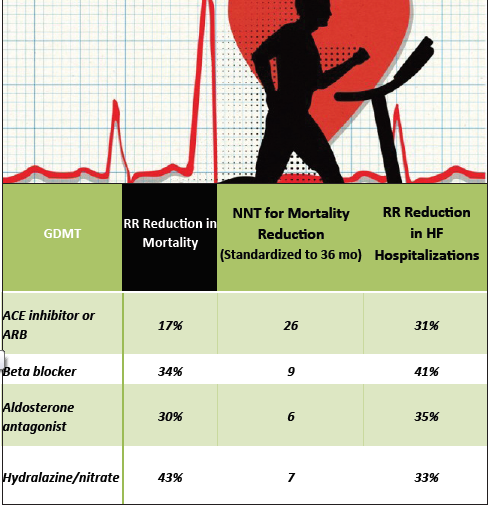
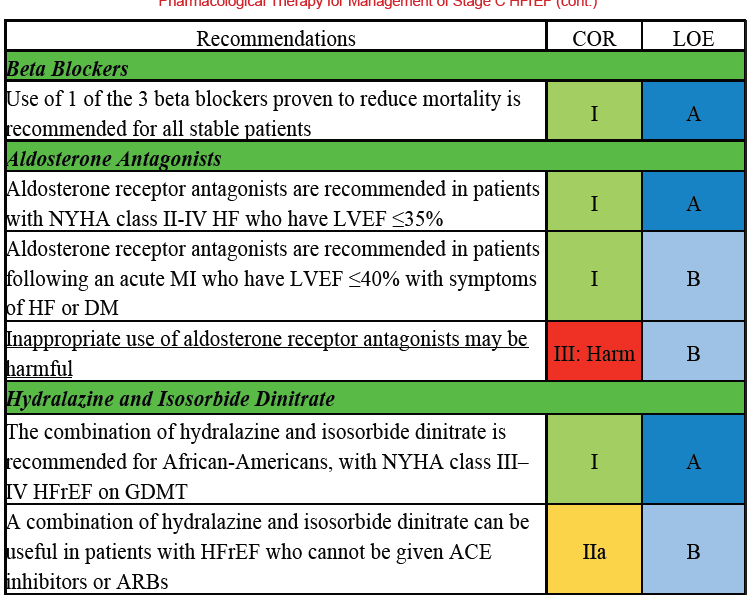
Farmacological Treatment
Systolic and diastolic blood pressure should be controlled in patients with HFpEF in accordance with published clinical practice guidelines to prevent morbidity.
Diuretics should be used for relief of symptoms due to volume overload in patients with HFpEF.
Coronary revascularization is reasonable in patients with CAD in whom symptoms (angina) or demonstrable myocardial ischemia is judged to be having an adverse effect on symptomatic HFpEF despite GDMT.
Management of AF according to published clinical practice guidelines in patients with HFpEF is reasonable to improve symptomatic HF.
The use of beta-blocking agents, ACE inhibitors, and ARBs in patients with hypertension is reasonable to control blood pressure in patients with HFpEF.
New treatment
Spironolactone
ConditionⅠⅠ
. Patient retuned back to his daily activities and continue on medical treatment including
- Ramipril 10 mg/day
- hydrochlorothiazide 12.5 mg/day
. being asymptomatic Patient after two years became
- non-compliant to treatment and life style
modification and he began to suffer from
. decrease his effort tolerance
. SOB on mild effort
. mild LL edema
. He sought medical advice
. Clinical examination revealed
- patient dyspnic at rest
- pulse 108/min , regular ,equal on UL &LL
- BP 158/116 mmHg
- LL oedema
- neck vein congested 12 cm
- cardiac apex in the 6th space out MCL
- S3 gallop
Physical Exam-Jugular Venous Distention
Technique for Measuring Jugular Venous Pressure
Patient reclining with head elevated 45°.
Measure elevation of neck veins above
the sternal angle (Lewis Method).
Add 5 cm to measurement since right
atrium is 5 cm below the sternal angle.
Normal CVP <= 8 cm H2O
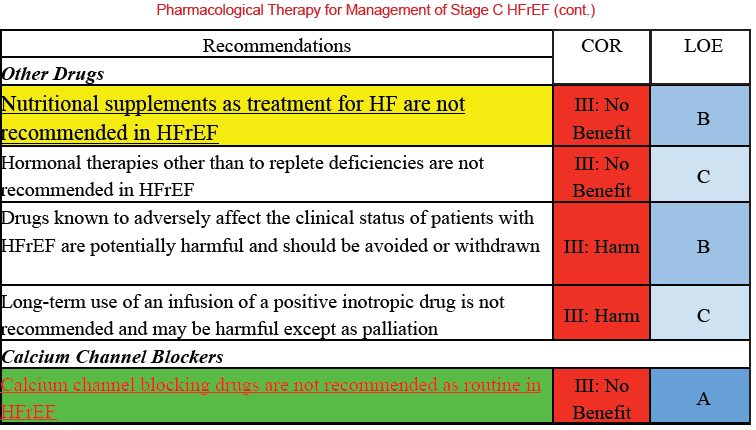
. The patient was admitted to the hospital where he received The following medication :
Ramipril 10 mg/day.
furosemide 40 mg /day
digoxin .25 mg once /day
isosorbide dinitrate 10 mg/day
multivitamins once/day ???
The following investigations were ordered
. New ECG
. X-ray chest
. echocardiography
. Blood urea and creatinine
. Echocardiography was done and it showed
EDD 6.5 cm
ESD 5.1 cm
IVS 1.2 cm
PW 1.3 cm
LA 4.6 cm
EF 34 %
. blood urea 38 mg/dl normal
. Creatinine 1.4 mg/dl normal
Questions
What Type of heart failure this patient did suffer ?
What is wrong in the management ?
Systolic Heart FailureHFrEF
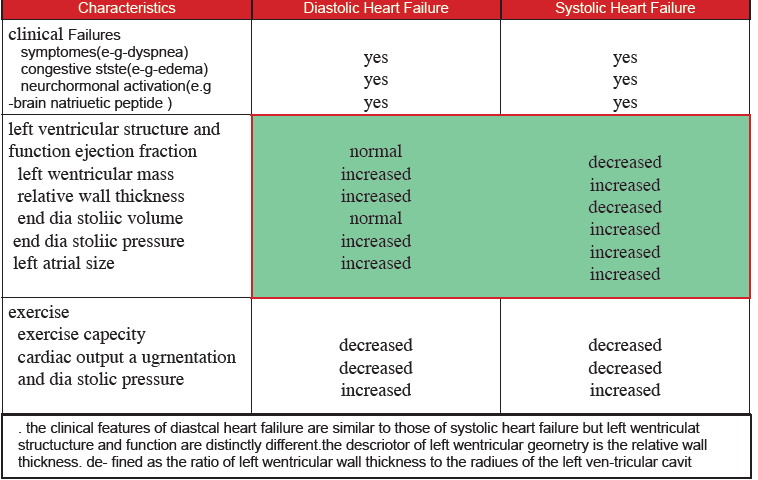
Characteristics of Systolic Heart Failure (HFrEF)
. Since the ventricle is inadequately emptied, ventricular end-diastolic pressure and volumes increase affecting the atrium.
. On the left side of the heart, the increased pressure is transmitted to the pulmonary vasculature extravasation of fluid into the lung parenchyma extravasation of fluid into the lung parenchyma pulmonary edema.
. On the right side of the heart, the increased pressure is transmitted to the systemic venous circulation and systemic capillary beds extravassation of fluid into the tissues of target organs and extremities dependent peripheral edema.
Ejection fraction drops below 40%.
. More readily recognized.
. Described as failure of the pump function of the heart.
Characterized by a decreased ejection fraction (less than 45%).
. The strength of ventricular contraction is attenuated and inadequate for creating an adequate stroke volume resulting in inadequate cardiac output.
. Caused by dysfunction or destruction of cardiac myocytes or their molecular components.
. Most common mechanism of damage is ischemia causing infarction and scar formation dead myocytes are replaced by scar tissue decreased function of myocardium causing wall motion abnormality.
Etiologies of Systolic Heart Failure
. Coronary Artery Disease (65%)
. Non compliant hypertensive patients
. Idiopathic dilated cardiomyopathy
. Alcohol/toxin-induced cardiomyopathy
. Infectious/inflammatory process
. Familial dilated cardiomyopathy
. Postpartum cardiomyopathy
. Stress induced cardiomyopathy
. Endocrine/nutritional causes . Tachycardia mediated cardiomyopathy
Final Clinical Pearls
. Heart failure is either Diastolic or Systolic Heart Failure.(HFpEF & HFrEF )
. EF is the main corner stone in the differentiation
We have to treat our patients according to recent guidelines
. Use physical exam and ancillary tests(BNP) to assess ADHF
. Tailor treatment based on clinical presentation.
. Follow guidelines when planning for disposition
. HF is a waxing and waning disease that is ultimately fatal


 info@utopiapharma.com
info@utopiapharma.com
 Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia
Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia