OCCUPATIONAL ASTHMA
OCCUPATIONAL ASTHMA
Dr٫ Mohamed M.Elbatanouny
Prof.of.Hospital Medicine
Cairo University
Definition of asthma :
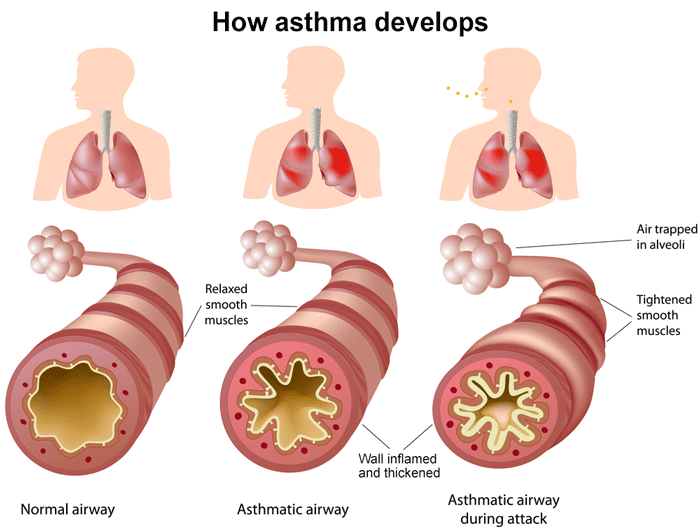
Is a pulmonary disorder characterized by widespread partial obstruction
of airways that is reversible ( completely or incompletely spontaneously or
as a result of treatment ), hyper-reactive airways, inflammation and airway
remodeling .
Occupational Asthma :
Airway obstruction follows workplace exposure to inhaled gases, dusts, fumes
or vapors which will acts as specific sensitizers and / or non specific irritants .
Prevalence of Occupational Asthma :
* Prevalence of asthma is 5% of the general population.
* Occupational Asthma prevalence varies between 2 -15% of asthmatic cases
in different countries .
* The relative incidence of allergic to non allergic asthma differ according to
type of industrial exposure, (e.g.: nonspecific respiratory irritation was the
cause of asthma in flour milling, baking and other flour based industries in
2.6% of workers while sensitization was responsible for only 0.3% of cases).
Risk factors of occupational Asthma:
Exposure characteristics : Chemical characteristics and
r.eactivity of the allergen. . Dose and intensity of exposure . The specific type of industrial
process ; asthma appears in about
5% with TDI, 10 – 40% with proteolytic
enzymes and 2 – 40% with grain dust
exposure.
.2- Geographical and climatic factors : Wind direction and humidity "
.epidemic . Cold environment " adverse effect
on exertion .
.3- Atopy : Atopic workers become sensitized
.more readily than do non atopic . Atopy is a predisposing factor in
case of exposure to high molecular
weight compounds (≥ 1000 daltons).
Examples: in enzyme detergent
manufacturing, laboratory animal
allergens and certain insect protein,
.Gum acacia and flour . If low molecular weight compound
(≤ 1000 dalton) is the cause
of asthma, atopy is not often a
predisposing factor.
Examples: in isocyanate
manufacture, western red cedar mills,
trimellitic anhydride (TMA), phthalic
anhydride (PA) and formaldehyde
.exposure. Nevertheless atopy may be
important in case of exposure to some
low molecular weight compounds .
Examples: Platinum salts, ethylene
diamine and dimethyl ethanolamine .
.4- Cigarette smoking : Cigarette smoking predisposes
.workers to allergic sensitization . There is a connection between
cigarette smoking and increased IgE
l.evel. Inhalation of cigarette smoke injures
the bronchial epithelial causing
widening of the tight junction between
epithelial cells that lead to increase
in epithelial permeability which result
great pene tration of antigen and
access to the immune machinery in
epithelium and vasculature.
5- Exposures to low level airborne
.workplace irritants. Cumulative lower level exposure
to airborne irritants may produce
bronchial epithelial injury and
consequences that are similar to
c.igarette smoking. Animal studies document that
antecedent exposure to an airborne
irritant (SO4, H2S, No2, O3, Cl2, NH3)
enhance allergic sensitization to an
.allergen . Human exposure to irritant gases
or dusts example (red cedar and
TMA) may lead to lower airway
inflammation which may then lead
to bronchial hyperresponsiveness.
It was hypothesized that higher prevalence of skin and bronchial reactivity among swimmers was due to frequent exposure to chlorine and its components in swimming pools.
6- Presence of non specific bronchial hyperresponsiveness.
. It occurs more commonly among young persons who may present with few symptoms or none.
. It occurs also among smokers with normal respiratory function and among highly trained athletes.
. These persons with hyperactive airways including asthmatics are more responsive to irritant.
7- Presence of sensitive subpopulations:
. A segment of the population appears to be more susceptible to develop workplace allergic sensitization because of certain host factors (atopy and smoking).
. Spontaneous mast cell degranulation is characteristic of asthma and some atopics (sensitive group). Perhaps mast cell degranulation is heightened after irritant exposure in this sensitive group.
. Airways of asthmatics and perhaps some atopic are leaky, the exudation of plasma into airways correlates with hyperresponsiveness to histamine and is decreased by corticosteroids.
. On the other hand airway hyperresponsiveness may lead to self protective decrease in exposure to dusty work environment and promote exclusion of them early from dusty work.
Immune or allergic asthma:
. Susceptible workers develop IgG and IgE antibodies .
. Susceptible workers secrete cytokines which evolve from the development of naive CD4+ T cells into functionally T subsets type (TH1 and type TH2).
. Atopy may be a predisposing factor to asthma if the responsible allergen is of high molecular weight ≥ 1000 dalton, Example, in enzyme detergents, animal and plant protein. In such cases atopics become sensitized more rapidly than non atopics .
. In low molecular weight compounds example, TDT and red cedar atopy is not often predisposing.
. A latent period between first exposure and onset of symptoms vary from weeks to years and is needed for sensitization to develop.
. The course of the disease will depend on the nature and severity of the immune response.
Classification of occupational asthma:
. On basis of offending agent
- Allergic (extrinsic asthma)
- Non allergic (intrinsic asthma)
. On basis of pathophysiology
- Reflex (neural)
- Inflammatory (epithelial damage by microbes or irritation).
- Pharmacological
- Smooth muscle hyperactivity
- Deranged B adrenergic system
- Immune
- B cell activity " IgE and IgG
- T cell activity " cytokine production
Characteristics of reflex asthma (reflex bronchoconstriction)
- Stimulation of irritant receptors
in airway wall by agents such as cold air, inert dust particles, gases and fumes .
- The reaction is non specific (not immune).
- Patient gives history of previous asthma and/or possesses abnormally reactive airway. For this reason, cases are often not accepted as asthma related to work exposure.
- Normally stimulation of ß-adrenergic receptors lead to activation of enzyme adenylcyclase which transform AMP into CAMP that cause bronchodilatation, while stimulation of cholinergic receptors activate guanylcyclase enzyme which transform GMP to CGMP that cause bronchoconstriction (look organic dust diseases)
Pathology of asthma.
. At autopsy, lungs are distended, bronchi and bronchioles are plugged with viscid tenacious mucous which contain excess eosinophiles, bronchial epithelial cells and Charcot- Leyden crystals, bronchial walls are thickened and edematous and mucous glands and smooth muscle cells are hypertrophied. This is actually the features of severe end disease.
. Biopsy specimens between active episodes in less severe cases may show disappearance of these structural abnormalities with the occurrence of recovery .
Clinical features of occupational asthma:
There are 2 types of asthma:
I- Occupational asthma without latency = irritant induced asthma = intrinsic asthma :
A- Reactive airway dysfunction syndrome (RADS):
Likely exemplified the extreme and of the spectrum of an irritant effect on the airways that is characterized by sudden onset (< 24 hours)
Example of causes of RADS are :
.Sulfuric acid/ SO2
.Smoke inhalation
.Locomotive diesel exhaust .
.Hydrochloric acid and chlorine gas.
.Ammonia fumes .
.Silo gas .
.Acitic acid .
.Zinc chloride (smoke bomb).
.TDI.
.Welding fumes .
B- Irritant asthma without so sudden onset:
. There is another form of irritant asthma that has not such sudden onset (develop ≥ 24 hrs ), irritant exposure is not so sudden or brief or massive, but continues for > 24 hours and initiation of asthma takes too larger time to evolve. It appears that :
- Pre exiting host susceptibility such as history of asthma or atopy may be a factor.
- Bronchial epithelial of atopic may react more to low level irritant than non atopic (due to hyperreactivity ) because of IgE linked to their surface.
Or Pre- exposure to irritants enhance airways sensitivity to allergens
II- Occupational asthma with latency period = allergic asthma = extrinsic asthma:
- Exposure to occupational allergen is followed by antibody production
- A latency period between first exposure and production of symptoms is necessary for sensitization to develop ; it varies from weeks to years.
- Allergic bronchoconstriction may occur immediately after exposure in already sensitized workers or may follow a delay of several hours or in a pattern with both early and late components .
A- Early-onset (immediate) asthma:
. Develop shortly after exposure, reach maximum in 10 – 20 minutes ends within 2 hours
. Sensitized worker have airway mast cells coated with IgE antibody. Inhaled antigen reacts with the specific antibodies (bridge them) causing mast cell to release mediators (type I reaction) which in turn cause bronchoconstriction and local inflammation with resultant cough, wheezing, airflow obstruction and dyspnea .
B Late onset (non immediate) asthma
. Begins sometimes after exposure and reach maximum at 4 – 6 hours and usually end in 24 hours.
. Recurrent nocturnal cough usually dry and dyspnea may be the only manifestation of occupational asthma and incorrect diagnosis of bronchitis is often entertained and usually the relation with exposure in such case is not obvious .
. The mechanism of late onset asthma is uncertain, it has been postulated that it may be due to :
- IgG antigen antibody complex
- Infiltration of bronchial epithelial by active eosinophiles and neutrophiles that cause bronchial inflammation and hyperactivity
C- Dual onset (combined asthma):
. The early attack resolves to be followed by hours later by a return of symptoms of bronchospasm .
. The key element influencing the pattern of symptoms and airflow obstruction are the recovery period and the effects of cumulative exposure.
. Some improve rapidly after leaving work with complete recovery by next day sush workers show similar changes during the shift
. Some other workers need > 2 days to recover. In such cases repeated exposure over several weeks result in steady deterioration of symptoms and pulmonary function.
. Symptoms and signs may be difficult to differentiate from those of chronic obstructive lung disease due to other causes.
. Some workers may show maximal deterioration of symptom on the first day of the week and recovery during the rest of the week day (Ex: in byssinosis)
Clinical features of occupational asthma:
Examples of occupational asthma
. Asthma due to cotton, flax, hemp or jute dust (Byssinosis)
- Cause of bronchoconstriction is not certain
- Dust extracts are capable of causing direct release of histamine and contain endotoxins from bacteria and fungi that can activate the complement system
- Dust extracts contain also histamine, serotonin and unknown constrictor factor
- Precipitating IgG antibodies are found in exposed workers more in those with chest tightness and type III reaction has been postulated or being only an index of exposure was also suggested.
- Symptoms begin occasionally on first day of the working week or after vacation (Monday fever) and abat during the week.
- Progressive removal of antibody or depletion of chemical mediators may explain this pattern of asthma.
- Time away from work allows their antibodies and mediators to gain higher levels on the 1st day of working week.
- A latent period of 10 years is needed for the symptoms to appear and may be less than that. Condition may proceed to chronic bronchitis and permanent disability.
. Asthma due to grain dust
- Dust is a mixture of grain proteins,
Some causes of allergic asthma
- Animal dander
- Antibiotics, sulphonamides, azodyes
- Bacillus subtilis enzyme (in washing porders)
- Flour dust
- Green coffee or tea dust
- Caster bean
- Spice (garlic powder)
- Enzymes (pepsin, pectinase, trypsin)
- Maple park and African zebrawood, western cedar wood
- Phthalic anhydride and other anhydrides & TDI.
- Complex platinum salts
- Gum Arabic
- Marine and fish products
fungi, insects, bird and rodents excreta.
- Dust in an irritant and also can activate complement
and release histamine so it can cause reflex and allergic
immediate and late asthma.
- The complex composition of dust makes it difficult to
identify the specific antigen.
- Fever and leucocytosis sometimes accompany late
asthmatic reaction.
- Skin test results with grain dust extract is equivocal (not
sensitive and not specific) . Asthma due to wood dust: e.g. western red cedar
- Contain a low medullar weight plicatic acid which
possesses both irritant property causing reflex asthma
and rhinitis. Also when conjugated with human serum
albumin, can elicit specific IgG and IgE antibodies causing
late and dual asthmatic pattern .
- Recurrent nocturnal attacks are common presentation
of late reaction and thus the relationship with exposure
may be missed. . Asthma due to acid anhydrides:
-. Acid anhydrides include: . Phthalic anhydride (PA) . Hemic anhydride (HA) . Maleic anhydride (MH) . Trimellitic anhydride (TMA) And others . Asthma due to metal salts
- Exposure to complex salts of platinum after conjugation
with human serum albumin (PHSA) can elicit IgE
antibodies " immediate asthma.
- Platinosis a triad if asthma, urticaria and rhinitis was
frequently encountered.
- Other metals such as nickel, chromium, cobalt,
vanadium and tungsten carbide can cause asthma but the
mechanism of the reaction is not known. . Asthma due to isocyanates:
- There are 2 different groups of commercially important
isocyanates :
1) Aromatic isocyanates . TDI (toluene diisocyanate): low molecular weight,
volatile substance . MDI (methylene diphenyl diisocyanates): less volatile
than TDI and therefore less toxic . NDI (naphthaline diisocyanate)
2) Aliphatic diisocyanate:
HDI (hexaethylene diisocyanates) volatile substance such
as TDI . Isocyanates are important intermediaries in the
production of urethane by reaction between amines and
phosgene . Urethane reacts with polyglycols to form polymeric
mass and if H20 is added CO2 is evolved and foam is
produced . Single episode of isocyanate exposure may lead to
acute or long lasting effects including:
- Irritant effect causing lung injury
adult respiratory distress syndrome (ARDS)
characterized by:
1) Diffuse alveolar damage (if exposure is overwhelming)
2) Dyspnea and hypoxemia
3) Acute mortality risk
4) Chronic physiological impairment sequelae
- Breif excessive exposure will lead to reactive airway
dysfunction syndrome, (RADS) due to stimulation of C
fibers. . Sensitization may develop leading to production of
asthma which occurs in 5 – 10 % of workers (small %)
and characterized by:
- Exposure may be excessive or of low conc. < 0.001 ppm
- May present with acute, late or dual asthma
- Typically asthma begins near the end of the working
day and continued through night, improving somewhat in
the morning hours and then recurring in similar temporal
fashion following the next working day
Diagnosis of asthma:
To confirm the diagnosis of
occupational asthma we must
identify the cardinal features of
asthma as well as the feature
of work relatedness: .Verify the symptoms and signs of asthma:
- Classic symptoms are dyspnea,
chest tightness and wheezing
- Non classic S. & S. " recurrent
attacks of bronchitis with sputum and
rhinitis which may begin late (hours
after exposure has ceased).
- In some patients recurrent nocturnal
attacks of dyspnea and cough may be
the only complaint.
- Detailed occupational and
environmental history and accurate
medical and respiratory history to
exclude past history of asthma or the
presence of non occupational related
pulmonary conditions. .Complete physical examination:
Examination of worker may show
no signs and so examination should
be done during exposure at work.
Wheezing may be detected by
auscultation and difficulty in breathing
may be evident, exclusion of non
occupational pulmonary disease is
important. . Documentation of reversible air
flow limitation and its relatedness
- Diurnal variation of FEV1≥ 20%
between 8 AM and 4 PM.
- Work relatedness changes in FEV1
or PEFR $ more than 25% during shift.
- A reduction in PEFR measurement
at work and not at home confirm
reversible work related
bronchoconstriction, enough time
for recovery and response must
be considered. Therefore multiple
recording are recommended for 2 – 3
weeks at work and least 10 day off
work.
- Stop resume work test (symptoms
recur on resuming work).
- Confirmation of specific airway
hyperresponsiveness by specific
inhalation challenge test. The test
should be done in hospital since late
reaction can occur after challenge and
may be severe and require urgent
treatment.
- Preferable confirming non specific
airway hyperresponsiveness by
methacholine, histamine or carbacol
inhalation challenge. . N.B: Absence of positive non specific airway hyperresponsiveness test does not rule the diagnosis of asthma
. Document the immune sensitization for allergic cases
- Prick skin testing is not sensitive or specific
- Detecting IgE using (RAST) radioallergosobent test
- Detecting IgG and/or IgE using enzyme linked immunosorbent assay (ELISA)
- Use of complement fixation tests, precipitating antibody assays and lymphocyte tests
- Monitoring blood and sputum eosinophilia which are markers of allergic process. Often ≥ of 15% sputum cells are eosinophils in asthmatic patient
- Stop resume work test can help to differentiate occupational from non occupational asthma (number of eosinophiles decrease both in blood) and sputum when away from work for several days. (Eosinophile level is rough estimate of severity of the attack).
Prognosis of occupational asthma:
- The most aggravating factor for occupational asthma is continued exposure to the antigen to which the person is sensitized.
- Irritant and physical triggers do not cause asthmatic attack but may exacerbate asthma if present.
- Persistence of asthma after termination of exposure is common (50 – 90%) of cases and is best documented for isocyanate and western cedar asthma.
- Following termination of exposure, clinical improvement of asthma may occur concurrent with reduction in airway non specific hyperactivity may persist.
- Inhaled corticosteroid improves the clinical and functional recovery from occupational asthma.
. The following environmental factors retain potential or permanent aggravators for asthma:
* In door home allergens e.g.pests, cockroach, fungi contaminating humidifiers and conditioning systems
* Outdoor allergens e.g pollens and fungi
* Active and passive smoking especially for children
* Drugs and food additives e.g. aspirin
* Community air pollution e.g. SO2, O3, NO2
* Viral respiratory infection
* Exercise hyperventilation (change in bronchial fluid osmolarity)
* Emotional stress (hyperventilation and hypocapnia)
. The determinates of unfavorable prognosis of asthma are:
* Longer duration of exposure and symptoms before diagnosis
* Development of dual response after specific inhalation challenge
* Finding of airway obstruction at time and study
* Persistence of markers of inflammation in BAL and biopsy
* Rapid than normal annual decline in pulmonary functions
Prevention of occupational asthma:
1)- Removal of sensitized worker from exposure because:
* Low exposure below P.L may cause a serious asthmatic reaction.
* Repeated low level of exposure can lead to irreversible airway obstruction in those workers.
* High concentration of the material (such after accidental spills) may cause non allergic asthma and possibly death from severe asthma reaction.
2)- Substitution of another agent for the one that cause sensitization or alteration of the manufacturing process such as washing or steaming of cotton before its early processing which reduce disease (byssinosis).
3) - Engineering dust and vapor suppression.
4) - Medical surveillance program directed to the early detection of disease and identification of those at risk by periodic medical examination, periodic spirometric and peak flow survey and immune state monitoring.
5) - The question of atopy and bronchial hyperactivity as a pre-employment screening tests for exclusion from work or employment is not yet settled.
6) - Avoidance of trigging factors at home and in outdoor environment is also important.
7) - Smoking cessation program is also indicted
1)- Preventing or minimizing asthma through therapy should not take preference over preventive measures that reduces airway inflammation such as removal from allergen exposure or trigger situations
2)- Medication can be divided into:
a. Controller type medication taken daily on long term basis
I. Anti inflammatory drugs e.g., corticosteroids inhalation
II. Mast cell stabilizer e.g., cromolyne Na inhalation
III. Long acting bronchodilators (inhaled ß-adrenergic stimulants or xanthins)
IV. Use of zaditen: A long acting antihistaminic and mast stabilizer drug
b. Quick relievers (I.V)
I. Short acting bronchodilator
II. Short acting antihistaminic
III. Short acting corticosteroids
Quick relievers inhibit bronchoconstriction but not reverse chronic Airway inflammation and airway hyperreactivity .


 info@utopiapharma.com
info@utopiapharma.com
 Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia
Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia