Pneumonia
What is Pneumonia?
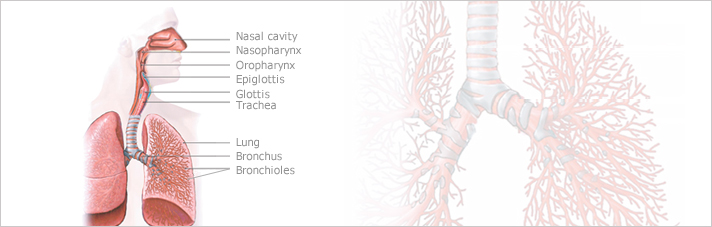
The lungs are a pair of breathing organs located within the chest.
Their function is to remove carbon dioxide from the air and bring oxygen to the blood. Pneumonia is a serious infection that affects the lungs. It is caused by viruses, bacteria, fungi, or the parasites, but most commonly pneumonia is caused by bacteria and viruses.
Community-acquired pneumonia (CAP) is an infection of the lungs that involves the small air sacs (alveoli) and tissues that surround them. CAP is a bacterial infection that is acquired in the community setting while other forms of pneumonia such as hospital-acquired pneumonia can be acquired while a patient is in a hospital or nursing home setting.
What are the risk factors of Pneumonia?
Factors associated with an increased risk of pneumonia include:
- Age. If you are age 65 or older, particularly if you have other conditions that make you more prone to developing pneumonia, you are at increased risk of pneumonia. Very young children, whose immune systems are not fully developed, also are at increased risk of pneumonia.
- Certain diseases. These include immune deficiency diseases such as HIV/AIDS and chronic illnesses such as cardiovascular disease,chronic obstructive pulmonary disease (COPD) and other lung diseases, and diabetes. You are also at increased risk if your immune system has been impaired by chemotherapy or long-term use of immunosuppressant drugs.
- Smoking, alcohol abuse.
- Hospitalization in an intensive care unit. People who need mechanical ventilation are particularly at risk because the breathing tube bypasses the normal defenses of the upper respiratory tract, prevents coughing, may allow the stomach's contents to back up into the esophagus* where they can be inhaled (aspirated), and can harbor bacteria and other harmful organisms.
- Having COPD and using inhaled corticosteroids for more than 24 weeks.
- Exposure to certain chemicals or pollutants. Exposure to air pollution or toxic fumes can also contribute to lung inflammation, which makes it harder for the lungs to clear themselves.
- Surgery or traumatic injury. People who have surgery or who are immobilized from a traumatic injury have a higher risk of pneumonia because surgery or serious injuries may make coughing — which helps clear your lungs — more difficult, and lying flat can allow mucus to collect in your lungs, providing a breeding ground for bacteria.
*The esophagus is the tube that carries food, liquids and saliva from your mouth to the stomach.
What causes Pneumonia?
Viruses and bacteria cause most case of pneumonia. The bacterial variety usually begins suddenly and often develops during or after upper respiratory infections. Parasites and other organisms can cause pneumonia to develop as well, and so can some allergies.
Aspiration pneumonia can develop if a person inhales powdered medication, food, vomit, or mucus into the lungs. Inhaling infected air can be the cause of pneumonia if a person has a weak immune system. Therefore, children and elderly people are at higher risk for pneumonia than healthy younger people.
Streptococcus pneumoniae is the most common bacterium which causes Community-Acquired Pneumonia (CAP). Haemophilus influenzae and Moraxella catarrhalis also cause CAP. Atypical pathogens such as Legionella pneumoniae, Chlamydia pneumoniae and Mycoplasma are recognized as important as they also cause CAP in both young and elderly patients. A variety of viruses, such as influenza occurs in association with CAP and usually precedes the pneumonia. Groups at high-risk for acquiring CAP include the elderly as well as individuals who smoke
What are the symptoms associated with Pneumonia?
Most people who develop pneumonia initially have the symptoms of a cold.
This is followed by a high fever (sometimes as high as 38.3° Celsius), shivering with chills, and cough with sputum production. Patients may become short of breath. Chest pain may develop if the outer aspects of the lung are involved. For some people with pneumonia, coughing is not a major symptom because the infection is located in areas of the lung away from the large airways.
- Fever
- Cough
- Shortness of breath
- Sweating
- Shaking chills
- Chest pain that fluctuates with breathing (pleurisy)
- Headache
- Muscle pain
- Fatigu
-
How is Pneumonia diagnosed?
Diagnosis of pneumonia is usually made from a medical history, physical exam and chest X-ray. The chest X-ray is done to look for changes in the lungs that may indicate pneumonia, other causes of symptoms, or complications of pneumonia. However, pneumonia that develops within 24 hours, along with severe dehydration or an indication of low white blood cell count, can hardly be detected by a chest X-ray.
There are the several other exams available :
A sample of the sputum can be incubated and the offending bacteria can be subsequently identified. A blood test can measure the white blood cell count. In up to 50% of the cases, the organism (such as bacterium or virus) that is causing the pneumonia infection is not identified even with those tests.
-
How is Pneumonia treated?
-
Primarily antibiotics are used for the treatment of bacterial pneumonia. The doctor will base the prescription on the medical history, a physical exam, age, other symptoms, and degree of severity.
Oral antibiotics are taken for 1-2 weeks, but a longer time may be needed for children or elderly people. Between 50% and 90% of pneumonia patients may be treated as outpatients. These patients usually respond well to the latest oral antibiotics.
Pneumonia patients usually do not need a special diet. Generally the treatment requires the patient to drink lots of liquids, use a humidifier,and get extra oxygen if necessary.
Patients may need to apply a hot pack to reduce chest pain and take a non-steroidal antiphlogistic. The patient needs to spit out the sputum when coughing; therefore, no cough medication is prescribed.
When coughing interrupts sleep, a cough medicine may be used. Medications for headache and fever may be used. When patient has difficulty in coughing up sputum, an expectorant can be used to dilute the sputum and aid in its elimination.
.

 info@utopiapharma.com
info@utopiapharma.com
 Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia
Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia